Retinopathy, a common eye disease, holds the potential to cast a shadow on one’s visual world. The intricate web of blood vessels within the retina, responsible for capturing and transmitting images to the brain, becomes compromised in this condition. Often associated with diabetes, retinopathy silently progresses, posing a significant risk to vision if left undetected and untreated.
In the realm of ophthalmology, the early detection of retinopathy is of utmost importance. Diabetic eye screening plays a vital role in identifying and monitoring the development of this condition. By examining the retina using advanced imaging techniques, ophthalmologists can uncover the subtle signs and symptomatic patterns that mark the presence of retinopathy. Prompt diagnosis can lead to timely interventions, preserving the precious sense of sight.
Retinopathy, though often tied to diabetes, is not an isolated concern. It shares a close relationship with another formidable eye disorder – glaucoma. These conditions can manifest independently or, in some unfortunate cases, concurrently, making the accurate identification and differentiation between the two crucial. Understanding the distinct features and progression of both diseases empowers ophthalmologists to guide patients towards informed choices and personalized treatment plans.
As we delve deeper into the realm of retinopathy, we will uncover the mechanisms behind its onset, the risk factors that predispose individuals to its development, and the available management options. Our journey will shed light on the importance of regular eye screenings, not only for those with diabetes but for individuals at risk of glaucoma as well. Embark on this exploration as we endeavor to unmask the reality of retinopathy, empowering individuals to safeguard their vision and see through the shadows with clarity.
Understanding Retinopathy
Retinopathy is a condition that specifically affects the eyes, falling under the realm of ophthalmology. It is commonly associated with individuals who have diabetes, as it is often a consequence of the disease. One of the key aspects of managing retinopathy is through regular diabetic eye screenings. This important procedure allows healthcare professionals to identify any signs of retinopathy promptly.
When left untreated, retinopathy can lead to more severe complications such as glaucoma. Glaucoma is a condition characterized by increased pressure within the eye, which can cause damage to the optic nerve. Therefore, it is crucial to monitor and address retinopathy to prevent it from progressing to this advanced stage.
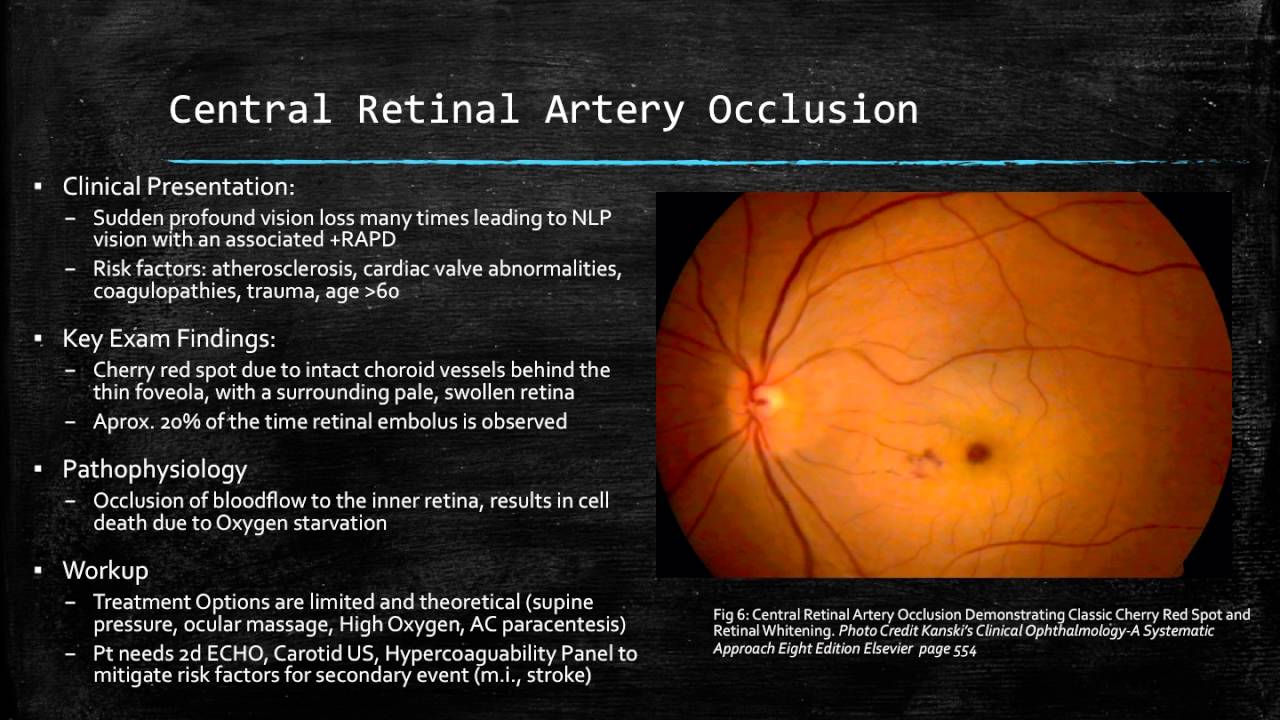
Retinopathy occurs when the blood vessels in the retina, the light-sensitive tissue at the back of the eye, become damaged. This damage is often a result of high blood sugar levels over an extended period, which can cause the blood vessels to weaken and leak. As the condition progresses, new blood vessels may grow in an attempt to compensate for the damaged ones. However, these new vessels are often abnormal and fragile, leading to further complications.
In summary, retinopathy is a condition linked to diabetes that affects the blood vessels in the retina. Regular diabetic eye screenings are essential to detect and manage retinopathy early on, preventing it from progressing to more severe conditions such as glaucoma. It is vital for individuals with diabetes to prioritize their eye health and work closely with healthcare professionals for effective management and treatment of retinopathy.
Diabetic Eye Screening
Diabetic eye screening plays a crucial role in the early detection and prevention of vision problems associated with retinopathy. As individuals with diabetes are at a higher risk of developing this condition, regular eye screenings become essential for maintaining optimal eye health.
During a diabetic eye screening, ophthalmologists conduct a comprehensive examination of the eye to assess its condition and identify any signs of retinopathy. This examination typically involves the use of specialized instruments and techniques, allowing for a detailed evaluation of the retinal blood vessels and other structures within the eye.
Early diagnosis of retinopathy is vital in preventing its progression and minimizing the risk of vision loss. By detecting this condition in its early stages, medical professionals can implement appropriate treatment strategies and lifestyle interventions to manage and control the disease effectively.
Moreover, diabetic eye screening is not only focused on detecting retinopathy, but it also helps identify other eye conditions such as glaucoma. This comprehensive evaluation ensures that individuals with diabetes receive effective and timely care to preserve their vision and overall eye health.
In summary, diabetic eye screening is a vital component of managing retinopathy and other eye conditions in individuals with diabetes. By regularly undergoing these screenings, patients can receive early detection and intervention, leading to better outcomes and a reduced risk of vision loss.
The Link Between Retinopathy and Glaucoma
Diabetic eye screening
Retinopathy and glaucoma are two prevalent eye conditions that can have a significant impact on an individual’s vision. While they are distinct conditions, there is a clear link between the two.
In retinopathy, the blood vessels in the retina become damaged due to various factors, most commonly diabetes. This damage can lead to leaking or bleeding of the vessels, affecting the overall health of the retina. On the other hand, glaucoma is characterized by increased pressure within the eye, which can damage the optic nerve and result in vision loss.
The link between retinopathy and glaucoma lies in the fact that both conditions can often occur concurrently in individuals. Research has shown that individuals with retinopathy are at an increased risk of developing glaucoma. This is believed to be due to the shared underlying risk factors and mechanisms that contribute to the development of these conditions, such as high blood pressure and abnormalities in blood vessel structure and function.
Furthermore, the presence of retinopathy can complicate the management of glaucoma. In cases where retinopathy has caused damage to the blood vessels in the retina, it can affect the accuracy of certain diagnostic tests used in glaucoma assessment. Thus, it becomes crucial for healthcare professionals to consider the presence of retinopathy when evaluating individuals for glaucoma and to adapt their approach accordingly.
In conclusion, while retinopathy and glaucoma are distinct eye conditions, there is a clear link between them. Individuals with retinopathy are at an increased risk of developing glaucoma, and the presence of retinopathy can complicate the management of glaucoma. Understanding this link is essential for effective diagnosis, treatment, and ongoing care for individuals with these conditions.